An Overview Of Primary Headaches
There’s perhaps no medical terminology/condition— save for the “malarias,” and the “typhoids“—as abused as “migraine” by the uninitiated. Migraine has come to mean different things to different people: for some, it is any headache that is “severe” and perhaps incapacitating. To others, it is any headache that recurs habitually. With this loose definition of the term migraine, the fact is that many headache syndromes labelled as “migraines” are not actually migraines. In this article, we will be looking at the different types of primary headaches, including those often mistaken by the uninitiated as “migraines,” and the typical migraine headaches.

Headaches: Primary Vs. Secondary
Headaches are broadly classified into Primary and Secondary forms.
- Primary headaches are headache syndromes which are disease entities of their own; they are usually nor caused by some other illness.
- Secondary headaches are those that arise as part of the symptoms of another illness; they are therefore caused by a readily identifiable local, or systemic illness. Example of causes of secondary headaches include; – Malaria – Typhoid – Hypertension – Sinusitis – Brain tumour – Meningitis – Brain bleed. – Etc.
Primary Headaches and Migraine
Primary headaches, as hinted above, are headache syndromes of their own, with no known systemic, or readily identifiable local cause.They are usually responsible for moderate, to severe, nagging headaches that keeps on recurring. Due to their habitual recurrence, they are likely to be what people have when they make statements such as this:”Headache is MY USUAL sickness.” Also, because of how severe and debilitating they can be, they can be easily mistaken for migraines, especially by the uninitiated.Headache syndromes that fall into this category include;
- Migraine Headaches
- Cluster Headaches
- Tension Headaches
Migraine
Migraine is more than just headaches: it is a complex neurological disorder usually characterized by warning signs—called prodrome or aura, which culminate in a moderate to severe headache with characteristic features.Migraines are commoner in adolescents and young adults— especially those that are females. As a rule of the thumb, any headache that started after age 40 to 50 is UNLIKELY a migraine headache.It is important to note that what makes a headache a Migraine headache, or not, is not the severity of the headache, but its UNIQUE characteristics.
Recognizing A Migraine Headache:
Migraines are usually characterized by the following features:
- A moderate to severe headache.
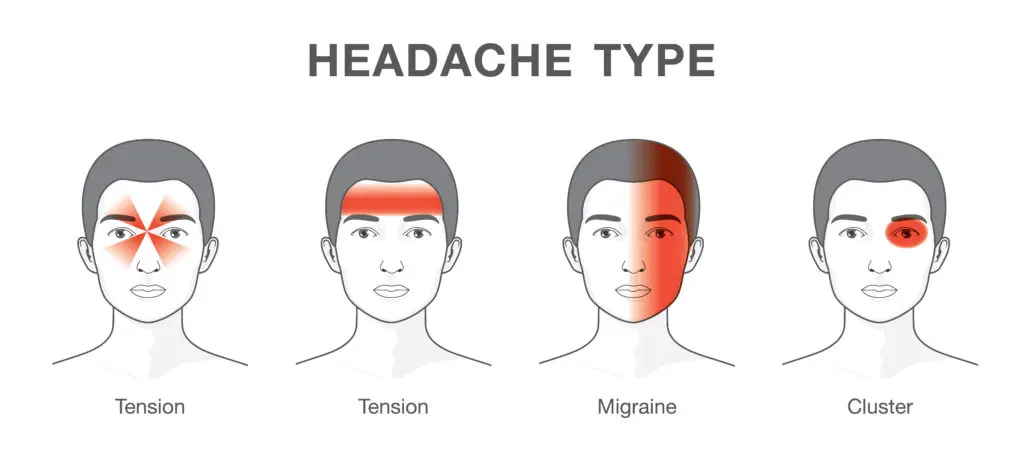
- Headache is usually one-sided. That is, it usually involves just one side of the head, and face [can involve the two sides in some cases, though]. Areas usually involved are the forehead, the sides of the head, and sometimes the neck.
- Headache is usually pulsatile or throbbing.
- It is worsened by physical activity: a sufferer would prefer to lie still as even the slightest physical exertion may worsen it.
- It may be accompanied by redness of the eyes, and aversion to bright light, and or sound.
- It may be accompanied by nausea, and or vomiting.
- An episode typically lasts about 4 to 72 hours.
- It may come with a premonition, in the form of mood changes, loss of appetite, or nausea.
- It is usually preceded by an aura, in some patients. The aura may come as billows of coloured lights, or black spots, in the field of vision. .If your Headache does not have at least 70% of these features if is UNLIKELY a Migraine.
Risk Factors For Migraine
Factors that predisposes one to developing a migraine, or that may trigger an attack, include:
- Drinking of alcohol, especially red wine.
- Flashes of light
- Rapid weather changes
- Skipping of meals – Stress
- Menstruation
- Oral contraceptive pills.
Variants Of Migraine HeadacheThese are forms of migraine which— in addition to the symptoms mentioned in the main post— may also come with atypical features. They include:
- Hemiplegic MigraineIn which one may be paralyzed on one side of the body during the attack.
- Ophthalmoplegic MigraineIn which one may have paralysis of the eye muscles.
- Basilar MigraineIn which one may find it difficult to talk may have ringing in the ears, and problem maintaining balance.
Prevention, And Treatment of Migraine
- Avoiding the aforementioned triggers as much as possible may help in preventing Migraine attacks.
- For people with frequently recurring episodes, oral medications like Beta Blockers, Calcium Channel Blockers, and TCAs, may be used as prophylaxis.
- Mild to moderate attacks can be treated with common analgesics, including NSAIDs, while severe attacks may be treated with Ergot alkaloids, and Triptans.
CLUSTER HEADACHES
These are about the most painful of the primary headaches, more painful than the migraines! As a matter of fact, some schools of thought have it that Clusters may be one of the most painful — if not THE most painful—medical conditions! The distinguishing hallmark of Clusters is the presence of autonomic symptoms. Thus it is otherwise called Trigeminal AUTONOMIC Cephalalgia. Cluster headaches are commoner in young males, between the ages 20 to 40.
Recognizing A Cluster Headache:
Clusters, like Migraine, are usually one-sided. – Unlike Migraines, however;
- The pain is usually around the eyes and the temple. The patient may feel as if the eyes are being torn out.
- They don’t switch sides. This means that it usually keeps recurring on the same side of the face. Unlike migraines that can happen on one side of the face in a particular attack, and then on the other side in the next attack.
- Clusters last for a shorter duration of time— about 30 minutes to 3 hours. However, they may occur multiple numbers of times in a day.
- The sufferer feels restless, maybe pacing about, and may even feel like hitting the head on a wall, unlike in migraines where they prefer to lay still.
- Clusters following a diurnal variation and usually occur at night. – They are usually accompanied by autonomic symptoms on the same side of the face as the headache. This may include;
- Redness of the eye
- Tearing up
- Stuffiness of a nostril or a runny nose.
- Sweating on one side of the face
- Drooping eyelid, and narrowed pupil
- Clusters happen multiple numbers of times in a given period, say over 1 month to 3 months; then gives the patient a long duration of period, say 6 months to a year, without attacks. The attacks come in clusters, hence the name.
Variants Of Clusters Headache
- Chronic Paroxysmal Hemicrania – Hemicrania Continua
- Prevention, And Treatment
- Calcium Channel Blockers,
- Mood Stabilizers and Anticonvulsants may be used for prevention.
- NSAIDs may be used to relieve pain.
- Acute attacks however needs be aborted with Triptans, or Ergot alkaloids, or Oxygen therapy, or a combination of these.
TENSION HEADACHE
These are the commonest forms of primary headaches, and may even be the commonest cause of headache considering all aetiologies, including the secondary types.Tension headache is the headache you get when you’ve had a busy day, all stressed up, and perhaps didn’t sleep well.
Recognizing A Tension Headache:
- It is bilateral. This means that it usually involves the two sides of the head.
- It spreads across the forehead, the back of the head, and may also involve the neck, and shoulders.
- The sufferer feels a tightness in the head— like there’s a tight band tied across their head, or like there’s vice-like grip on the head.
- It does not possess any of the peculiar features described for the other two types of primary headaches.
Types of Tension Headache
- Episodic Tension Headache: Occurs usually after a stressful day, is mild and may resolve without treatment.
- Chronic Tension HeadacheOccurs almost daily, and is usually more severe.
Prevention, And Treatment Tension Headache
- Rest.
- Exercise.
- Good eating habit.
- Treatment is usually with the over-the-counter analgesics.
